Pros & Cons of Virtual Nurses in Healthcare
Pros & Cons of Virtual Nurses in Healthcare are increasingly shaping discussions about the future of patient care and nursing workforce models. As healthcare systems integrate digital technologies to improve efficiency and accessibility, virtual nursing has emerged as a transformative approach. Virtual nurses licensed professionals providing care through video communication, remote monitoring tools, and electronic platforms support clinical teams and enhance patient engagement.
While the advantages include improved workflow efficiency, expanded access to care, and enhanced monitoring capabilities, challenges such as limited physical assessment, communication barriers, and privacy concerns must be addressed. Understanding Pros & Cons of Virtual Nurses in Healthcare allows healthcare professionals, educators, and policymakers to evaluate how technology-driven roles can strengthen nursing practice without compromising patient-centered values.
Understanding the Pros & Cons of Virtual Nurses in Healthcare
Virtual nursing in healthcare refers to the delivery of nursing services through telecommunication technologies rather than direct physical interaction. These nurses collaborate with bedside teams and patients through digital platforms to provide education, monitoring, documentation, and coordination of care.
Healthcare organizations increasingly implement virtual nursing models to address staffing shortages, reduce administrative burden, and improve patient outcomes. However, evaluating the Pros & Cons of Virtual Nurses in Healthcare requires examining both practical benefits and potential limitations within clinical contexts.
Typical responsibilities of virtual nurses include:
- Admission and discharge support
- Medication education
- Chronic disease monitoring
- Care coordination
- Clinical documentation assistance
- Patient follow-up consultations
By focusing on communication-intensive tasks, virtual nurses enable onsite staff to prioritize hands-on interventions.
Benefits of Virtual Nurses in Modern Healthcare

Improved Workflow Efficiency
One of the most significant advantages of virtual nursing is the redistribution of workload. Bedside nurses often manage heavy documentation and communication responsibilities alongside clinical duties. Virtual nurses handle many of these tasks remotely, reducing time pressure and allowing onsite nurses to focus on direct patient care.
This collaborative model promotes productivity and can help alleviate burnout, a persistent issue affecting healthcare systems globally.
Enhanced Patient Monitoring
Remote monitoring technologies allow virtual nurses to track patient data continuously, including vital signs, symptom reporting, and treatment adherence. Early detection of abnormalities enables timely intervention, potentially reducing complications and hospital readmissions.
For chronic disease management, continuous digital monitoring strengthens continuity of care and supports patient safety.
Increased Access to Healthcare Services

Virtual nursing removes geographic barriers, allowing patients in rural or underserved areas to receive professional guidance. Telecommunication tools facilitate consultations that would otherwise require travel or extended waiting times.
This improved accessibility contributes to health equity by extending healthcare resources to populations with limited physical access to facilities.
Support for Nurse Well-Being
Workforce shortages and increasing patient loads place significant stress on nursing professionals. Virtual nursing models distribute responsibilities across teams, improving work-life balance and job satisfaction.
When administrative burdens decrease, bedside nurses can engage more meaningfully with patients, reinforcing professional fulfillment and retention.
Cost Efficiency for Healthcare Systems
Hospitals and healthcare organizations may experience financial benefits from implementing virtual nursing models. Improved patient monitoring can reduce readmission rates, while optimized staffing allocation enhances resource management.
Over time, these efficiencies may contribute to sustainable healthcare delivery models that balance quality care with operational costs.
Challenges and Limitations of Virtual Nursing
Restricted Physical Assessment
Despite technological capabilities, virtual nurses cannot perform tactile examinations or procedures. Physical assessments often require direct interaction to evaluate skin condition, mobility, or subtle clinical signs.
This limitation means virtual nursing must function as a complement rather than a replacement for bedside care.
Dependence on Technology Infrastructure
Reliable internet connectivity, functional hardware, and digital literacy are essential for virtual care delivery. Technical disruptions can interrupt communication and delay clinical decision-making.
Healthcare organizations must invest in robust infrastructure and training to minimize these risks.
Communication and Relationship Barriers
Nursing care extends beyond clinical knowledge; it includes empathy, therapeutic touch, and nonverbal communication. Virtual interactions may reduce emotional connection and hinder rapport-building between nurses and patients.
Maintaining compassionate communication through digital platforms requires specialized interpersonal skills.
Privacy and Data Security Concerns
Electronic handling of patient information introduces risks related to data breaches and unauthorized access. Strict cybersecurity protocols and ethical guidelines are necessary to safeguard confidentiality.
Nurses must also remain aware of regulatory standards governing digital healthcare interactions.
Ethical and Professional Considerations
Virtual nursing raises questions about accountability, role clarity, and equitable access to technology. Patients lacking digital resources may experience disparities in care availability.
Balancing technological integration with ethical responsibility remains an ongoing challenge for healthcare leaders.
Comparing Virtual Nursing and Bedside Care

Virtual nursing and traditional bedside care serve complementary functions rather than competing roles. Bedside nurses provide physical interventions, emotional reassurance, and direct assessments, while virtual nurses support communication, monitoring, and coordination.
Together, these roles create a hybrid care model emphasizing collaboration. Successful implementation depends on:
- Clear role definitions
- Interdisciplinary communication
- Adequate training
- Patient-centered integration
This collaborative framework highlights how evaluating the Pros & Cons of Virtual Nurses in Healthcare is essential to developing sustainable clinical systems.
Future Trends in Virtual Nursing Practice
As digital innovation continues, virtual nursing is expected to evolve significantly. Advancements may include:
- Artificial intelligence assisted decision support
- Enhanced wearable monitoring devices
- Expanded telehealth education training
- Virtual reality patient interaction tools
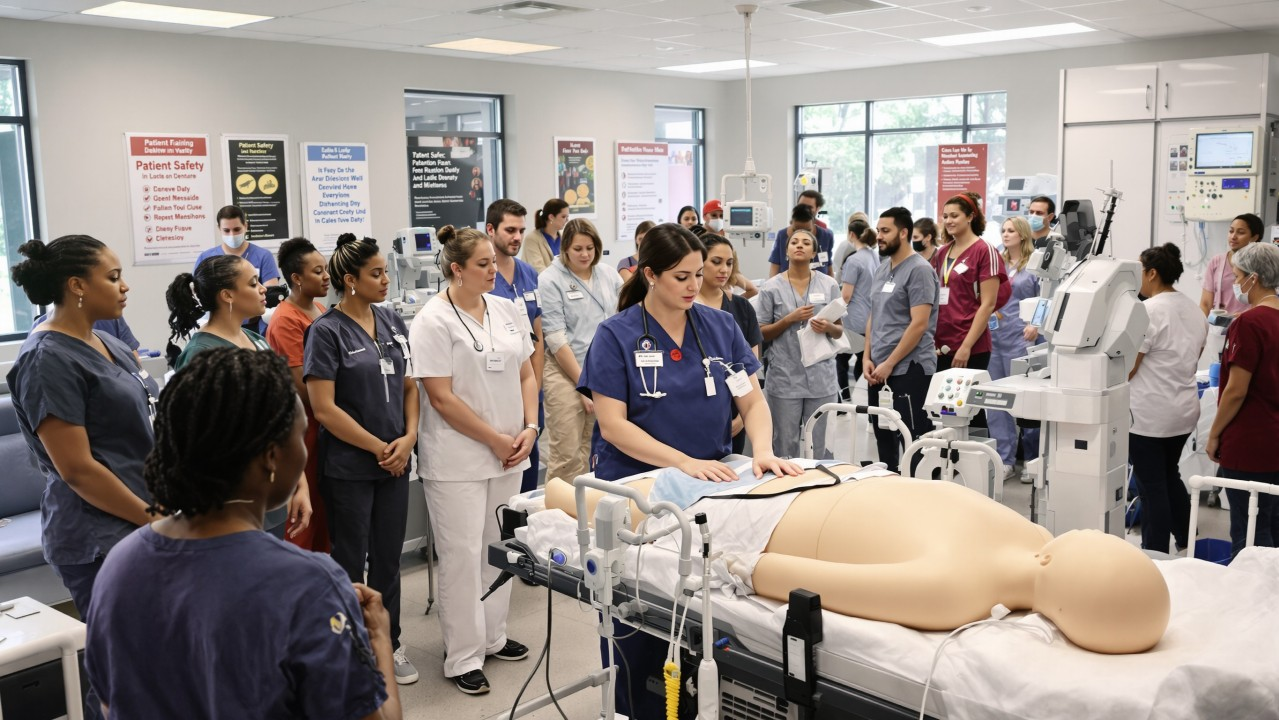
Nursing education programs are beginning to incorporate digital competencies, preparing graduates to function effectively in technologically integrated environments.
The future of healthcare will likely involve blended care models where virtual and in-person nursing intersect to maximize patient outcomes.
Conclusion
The Pros & Cons of Virtual Nurses in Healthcare reflect the broader transformation occurring within modern medical systems. Virtual nursing offers meaningful advantages, including improved efficiency, enhanced monitoring, expanded access, and workforce support. At the same time, challenges related to physical assessment limitations, technological dependence, communication barriers, and ethical considerations must be addressed thoughtfully.
Rather than replacing traditional care, virtual nursing represents an evolution of professional practice that integrates technology with human compassion. By recognizing both strengths and limitations, healthcare professionals can ensure that innovation strengthens rather than diminishes the core values of nursing.